North Carolina: Following Medicaid Expansion, Advocates Advance Medical Debt Protections
We have a medical debt crisis in this country.
It is a crisis that impacts more than 100 million people in the United States – that’s 4 in 10 adults. And we know it doesn’t impact everyone in the same ways due to historical and persistent injustices in our health system that make it harder for people, especially people with low incomes and Black and Latinx adults, to get affordable care.
At Community Catalyst, we have long advocated for local, state and federal action to address the medical debt crisis – shaping our health and economic justice policy priorities and powerbuilding strategy around the needs and desires of community leaders and organizations.
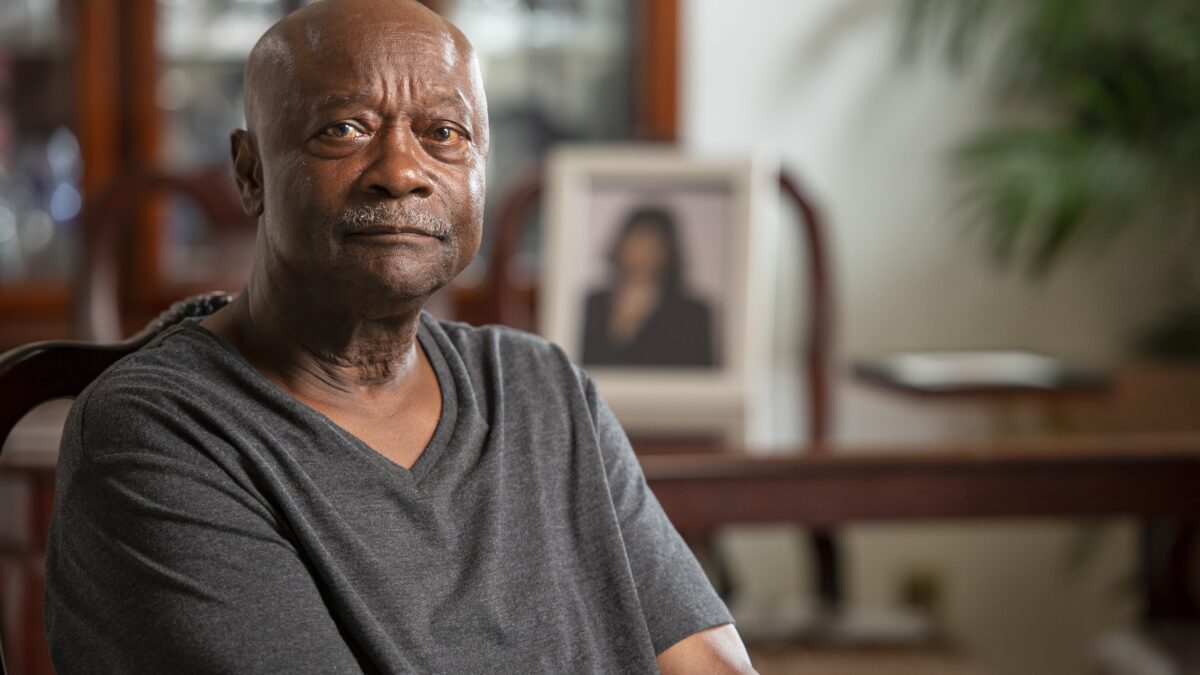
This is not some abstract policy debate that happens in Washington or Raleigh. It impacts real people. People like Terry Belk, a North Carolinian who has significant medical debt after both his and his late wife’s battles with cancer. Terry isn’t giving up, recognizing the power of our collective work to make a bigger impact.
I watched my wife die and these people still came at me, and her, as she was dying for money. Money we didn’t have. This is a national crisis… this is nationwide.”
We are proud of our shared accomplishments and recent progress made with the Biden-Harris administration to ensure medical debt doesn’t impact credit scores, but our progress doesn’t stop there. That is why the new medical debt relief incentive program in North Carolina is so exciting, as it represents the innovation and creativity needed to continue our work to deliver concrete solutions for people.
- The level of medical debt in North Carolina is high compared to the nation as a whole with evidence of inequity in how the debt is distributed.
- In 2022, 20% of North Carolina’s population had medical debt in collections, the fourth highest percentage among all 50 states. That figure increases to 25% for communities of color. In certain counties, the proportion of residents with debt in collection exceeds 40%.
The medical debt action taken in North Carolina, thanks to the leadership of Governor Cooper and on the heels of Medicaid expansion, provides immediate relief to individuals with medical debt and advances policies that tackle the root causes of the crisis, so that people don’t incur unnecessary debt in the first place or keep going back into debt simply for seeking needed care. Pursued by a state for the first time, this both/and approach incentivizes hospitals to participate through The Centers for Medicare & Medicaid Services’ Healthcare Access and Stabilization Program. North Carolina and the states that follow should make the program permanent.
“This is an innovative and exciting step forward in mitigating the harm medical debt is causing North Carolina families.”
This accomplishment would not have been possible without the tireless efforts of groups like the North Carolina Justice Center, a non-profit partner organization with a mission to eliminate poverty in North Carolina by ensuring that every household in the state has access to the resources, services, and fair treatment it needs to achieve economic well-being. Community Catalyst continues to partner with the NC Justice Center to:
- Push for permanent medical debt policies and protections that all hospitals must abide by, including legislative action to strengthen patients’ access to charity care (financial assistance), limit unfair debt collection tactics and restrict the ability of large medical facilities to charge unreasonable interest rates on medical debt.
- Connect the dots between Medicaid expansion progress with the medical debt crisis, recognizing that coverage alone is not enough, but will provide a pathway for more people to access affordable care.
Community leaders like Pastor John Jackman, who provided immediate medical debt relief to his parishioners in North Carolina while also advocating for policy change that addresses the underlying causes of medical debt, are also working to address the crisis.

“Medical debt is now a universal problem, no matter what your income level is… You can be pretty well off, have a pretty good job, and a long hospitalization can put you in debt.”
It is because of impacted people like Terry, community leaders like Pastor Jackman, and countless other advocates, that we will continue to advocate for solutions at both the state and national levels to end the medical debt crisis. Because the bottom line is: No one should have to exhaust their life savings or retirement accounts, or lose their housing because they went to a hospital to seek care.
North Carolina has taken a leadership role in this fight. We hope other states will follow.