Consumer Engagement: A Call for Tools that Measure Organizational and Policy Level Engagement
Everyone is talking about consumer engagement in health care. It is the term of art used to describe anything from reaching people through mobile apps, involving stakeholders in advisory groups to inform new program development, and even – in some circles – creating high-deductible plans so that consumers will have “skin in the game” and be “more engaged” in the management of health care by paying for more of their care. While the concept of consumer engagement appears to have many supporters, how the concept is defined and applied in practice, is less clear. Moreover, evidence-based strategies for successfully engaging consumer that are linked to clearly articulated and specific outcomes are few and far between.
Health care organizations are making significant investments in engaging consumers even though these efforts are not always leading to the engagement outcomes these organizations care most about. A case in point: A 2017 Change Healthcare study surveyed over 300 U.S. health plans and providers who reported that value-based care and competitive pressures have driven their investment in consumer engagement methods and technologies, with one-third of health care IT investment dollars being dedicated to consumer engagement. Yet, despite this significant investment, a majority of the nearly 800 consumers polled during the same Change Healthcare study period reported the quality of their experience with health plans and providers had declined or remained unchanged.
HOW CONSUMER ENGAGEMENT HAPPENS
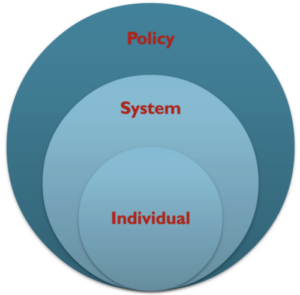
There are three levels at which consumer engagement can occur in the health care eco-system: system (i.e., during the policymaking process), organizational (i.e., health plan/ provider quality improvement strategies), and at the individual level (i.e., decision about one’s own health care). Engagement methods, particularly at the individual member level, typically center on non-participatory, one-way communication (i.e., patient outreach, patient education, electronic health care record access, etc.), and they are not often based on a well-defined strategy for obtaining desired engagement outcomes. Other engagement methods used in health care are characterized by symbolic participation (i.e., consumers have a voice through committees, but such committees may not carry weight with the powerful decision makers).
One of the few health care experts who have successfully defined, applied and measured consumer engagement head on is Dr. Judith Hibbard. Hibbard’s Patient Activation Measure (PAM) has been a rare and successful attempt at measuring consumer engagement at the health care member level, which has led to the tailoring of consumer engagement practices to address members’ health outcomes as well as community-wide health disparities. Even as greater numbers of health care organizations and large systems employ the PAM, a number of questions arise from her well-documented work: can we formalize and measure consumer engagement in areas beyond traditional medical care, for instance, in long-term services and supports and housing with service support models? Can we apply the lessons learned from Hibbard’s work to formalize and measure consumer engagement across the continuum of engagement that also includes organizational and broader systems improvement practices?
CONSUMER ENGAGEMENT AT THE ORGANIZATIONAL AND SYSTEMS LEVEL
Without a consistent definition of “consumer engagement” or standardized measurement, the ability to identify and adopt evidenced-based best practices at organizational and systems levels is challenging, if not impossible. Although we are not yet there, Laurie M. Jacobs and her colleagues make an important contribution to the field by publishing an inventory of tools for measuring engagement at the individual, organizational and systems levels. In addition to the PAM, they identify measures focused on the evaluation of consumer experience and satisfaction, and their components derive from a variety of sources including the Hospital Consumer Assessment of Healthcare Providers and Systems (HCAHPS) survey, the Medical Home Index: Adult, and self-efficacy measures like the Self-Efficacy for Managing Chronic Disease, to name a few.
While consumer engagement methods at the organizational level are diverse and include soliciting consumer feedback through surveys, advisory boards, and other evaluation strategies, the efficacy and results of this type of engagement remain unclear. As well, whereas toolkits on ‘how to engage’ can be used to inform the development of strategies within organizations, most focus on a wide range of elements that span committee composition, context and operational practice. It is therefore not surprising that even comprehensive tools that outline engagement factors, such as the Partnership Evaluation Levels and Measures framework, lack “credible evidence” to determine if engagement strategies work.
Even less is known about consumer engagement at the systems level. In many cases, consumers are underrepresented in broader policy and systems level decision-making, and because of that, standardized engagement methods and measurement practices are nearly nonexistent within this arena. We are left mostly with case studies and promising practices to inform consumer engagement in policy and systems work. Thus, even as measurement at the individual or direct care level is advancing, stakeholders (leaders, policy makers, researchers, etc.) need to pay heightened attention to the lack of meaningful definition and measurement of engagement at the systems level. This is especially true if the goal is to create a culture of engagement that permeates the entire delivery system.
That measurement gaps continue to exist have been noted by others, such as the National Quality Forum in its report on quality and home-based community services in support of community living. Ultimately, we need to address this void in measurement tools: given the investment that organizations are making to improve engagement, it would certainly be helpful to know if greater engagement is leading to the cost, quality, and health outcomes that these organizations are striving to achieve. Also, as others like Jacobs have duly noted, “…as consumer engagement continues to be an important consideration across multiple levels in our changing healthcare system, the ability to assess its impact, as well as short- and longer-term patient and system outcomes will be vital.”
Researchers and consumer advocate organizations alike are working to address the gap within applied practice and the literature by inventorying existing measures, developing comprehensive measurement frameworks, and seeking new ways to test measures’ validity. Only when engagement levers are firmly in place at all levels can we be certain that the basic infrastructure is there for a culture of meaningful consumer engagement and we can measure what, if any, effect consumer engagement has on quality, cost, and health outcomes.
Danielle Skenadore and Erin McGaffigan are Research Fellows at the LeadingAge LTSS Center and focus their research on evaluation, methods and outcomes associated with consumer engagement. Marc Cohen, Research Director at the Center for Consumer Engagement in Health Innovation, co-directs the LeadingAge LTSS Center @ UMass Boston. In this blog, they discuss progress to date and remaining gaps in defining and measuring engagement.