A Compendium of State Policies to Curb Hospital Prices and Reduce Medical Debt
16% Increase in health care prices from 2016 to 2020. As of 2022, over 100 million people in the U.S. are experiencing medical debt.
Explore state-by-state rankings >>
Read specific state policy summaries >>
State Spotlights
Some states stand out in Community Catalyst’s compendium with promising state policies to moderate hospitals’ prices and reduce medical debt. These states may also have the potential to be models for advocates and policymakers in other states. Explore the spotlighted states below.
Methodology
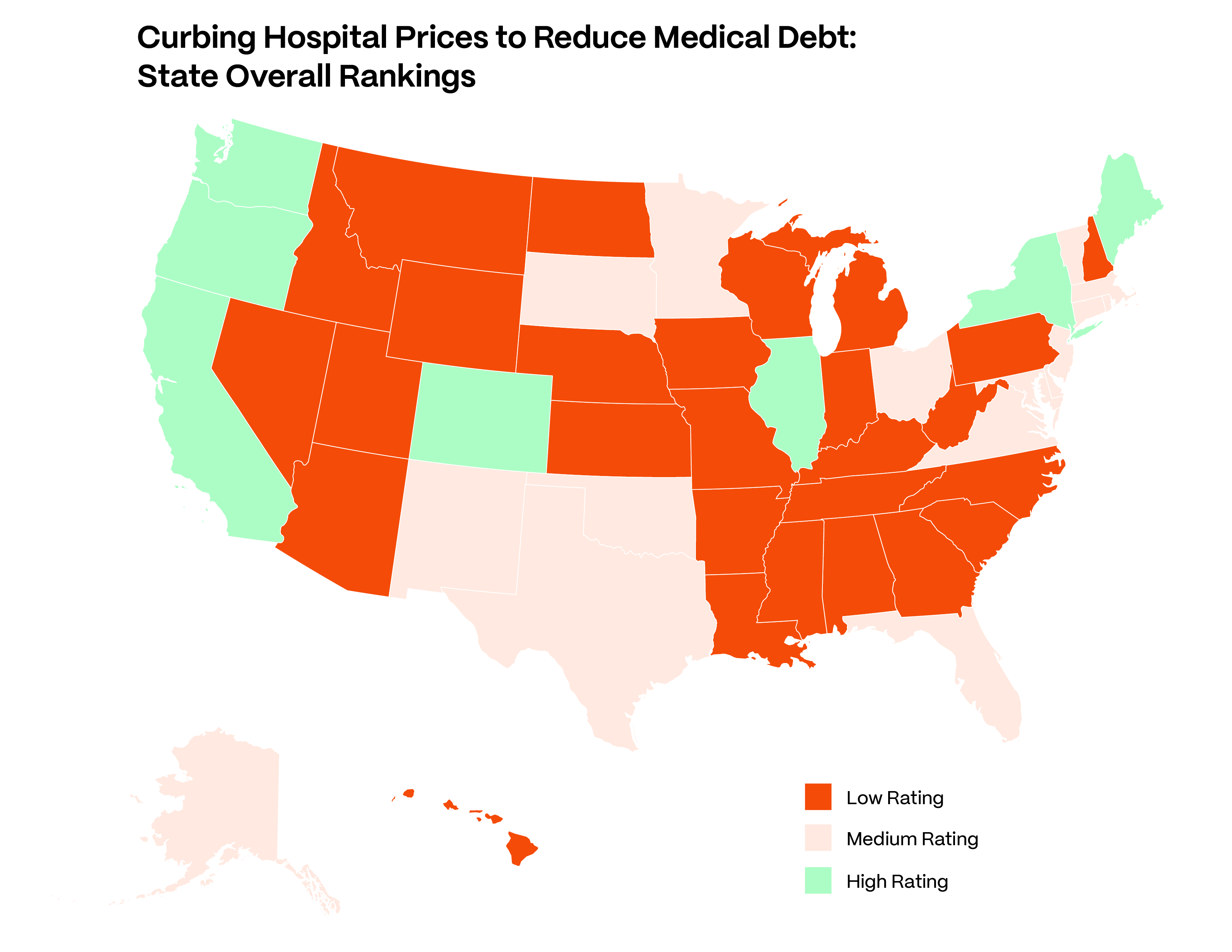
Community Catalyst identified five areas of policy that have the potential to reduce or grow medical debt, depending on any given state’s approach. The areas are financial assistance and free care, prescribed discounts/caps on charges, billing and collections, facility fees, and price transparency.
We rate a state’s policies in each of the categories as “low,” “medium,” or “high,” based on criteria including the scope of entities to which a rule applies, the specificity and extent of its requirements, and the strength of its enforcement mechanism. The ratings for each of the categories were then combined to produce an overall, composite rating for every state.

Introduction
The U.S. spent nearly $13,000 per person on health care in 2021. That is over 40% more than the next highest country, Switzerland, and nearly double the level in many other wealthy countries. Prices and the pursuit of profit are the primary reasons for this country’s high and rising health care spending. Yet, many hospitals today are thriving with non-profit and for-profit hospitals reporting increases in their mean profit margins. As prices rise, people take on more of the obligation to pay and bear the burden of health care and medical debts. We share some of the ways medical debt can impact people and how states can protect residents harmed by high hospital prices.
ConclusionConclusion
We have the most expensive health care in the world; as prices and debt continue to rise, further measures to protect individuals and communities are needed. Public policy is needed to help rein in soaring health care prices and reduce medical debt. The Compendium displays a range of state aggressiveness in policies that address hospital practices across several areas that affect prices and debt. Some states have exemplary policies, which seek to protect individuals’ rights, access, and pocketbooks, and which can serve as models for other states’ policymakers and advocates. For the states that lag behind, the Compendium can be used as a benchmarking tool and a reference guide to what is possible.
Read our conclusion brief to learn more about how we can reimagine policy levers that look beyond individual hospital behavior and towards systemic cost drivers like market consolidation and structural inequities.
Take ActionTake Action
States have the power to curb excessive hospital prices and protect patients from medical debt. Advocates can use the compendium to guide policy change that, at a minimum:
- Require all hospitals to provide free or discounted care to uninsured/underinsured patients with incomes under specified levels;
- Require all hospitals to limit the prices charged to patients below a specified income threshold to Medicare levels or lower;
- Require that hospitals screen patients for eligibility for free or discounted care, unless the patient specifically declines screening;
- Prohibit the most harmful collection actions, including wage garnishment, home foreclosures and property liens, adverse credit reporting, and denying medical care due to outstanding bills;
- Limit or prohibit facility fees;
- Require broad and accessible publication of hospital prices; and
- Robustly enforce all of these requirements, using, for example, financial penalties, licensure authority, and private rights of action.
This work was made possible by generous support from Arnold Ventures.
We thank authors Robert Seifert, Policy Researcher and Independent Consultant, Miriam Straus, Senior Policy Analyst at Community Catalyst, Sheila Philips, State Advocacy Manager at the Center for Community Engagement in Health Innovation, Michael Matson, Policy Analyst at Community Catalyst, and Quynh Chi Nguyen, Associate Director for the Center for Community Engagement in Health Innovation for their leadership in conducting state policy research and analysis.
We also thank Community Catalyst colleagues Brandon Wilson, Senior Director of the Center for Community Engagement in Health, Michael Miller, Senior Advisor of Strategic Policy, Amrit Cheng, Director of Storytelling and Content Strategy, and Karen Maniraho, Copywriter and Web Manager for their policy insight and content presentation.
