Hospital & Health Systems Accountability
Nearly 20 percent of people in the U.S. have medical debt, so it’s not surprising that a majority of people say that health care is unaffordable — with three-quarters giving U.S. health care affordability a D or F rating. The reality is, unaffordable health care and medical debt affects us all. And it’s an even greater burden for people from systemically excluded communities — including Asian, Black, Indigenous, Latinx*, and Pacific Islander communities.
What may surprise you is that hospitals and health systems frequently have financial assistance, billing, and collection policies that exacerbate existing inequities and leave millions of people with medical bills they cannot afford to pay. For example, there’s a common billing practice that requires a person without health insurance to pay a higher amount than a person with health insurance for the same procedure or exam. This creates a medical bill that is unlikely to be paid, leading to medical debt. It’s an endless cycle.
When it comes to non-profit hospital systems, it’s even more complicated. Non-profit hospitals are exempt from paying most taxes because they are supposed to operate for charitable purposes — as long as they provide a “community benefit.” Community benefit activities include things like providing free or discounted services to patients, education for health professionals, health research, and cash or in-kind contributions to groups in the community. But too often, this doesn’t happen at the level it should be happening, if at all.
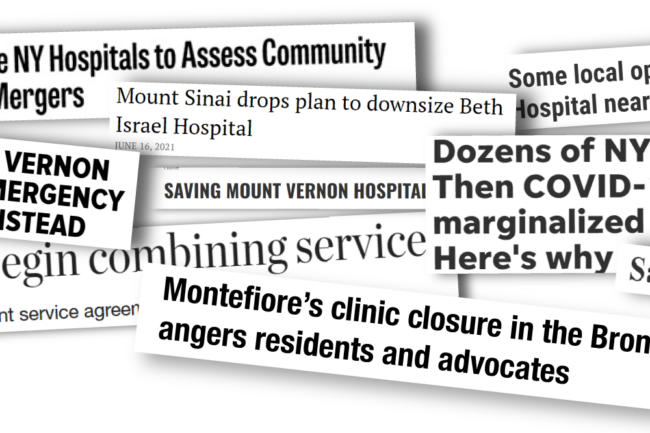
Surrounding all of this is the larger trend of consolidation in the health industry. Mergers and acquisitions of hospitals and health systems negatively impact communities as they stifle innovation and slow down progress towards value-based care. For example, consolidation eliminates facilities that are not religiously affiliated, which can create tremendous barriers to care for reproductive health care, including abortion.
Community Catalyst works with partners across a range of efforts designed to hold hospitals accountable to their communities, and shape practices and policies so that hospitals and health systems can better support the communities they serve — including through “community benefit” standards that actually respond to community needs.
Featured Work
Together with partners, we have pioneered new policy approaches and community organizing tactics to address hospital mergers, downsizing, and closings that are further depriving medically-underserved people and communities from access to essential medical services.
The Community Benefit and Economic Stability Project
We work with state and local partners in Colorado, Florida, Georgia, Illinois, Maine, New Mexico, New York, Pennsylvania, Wisconsin to develop community-driven financial assistance practices and billing and collection policies. We’re also involved in community engagement in health needs assessment to help hospitals better serve their communities and promote economic justice. This includes efforts to improve community benefit programming, hospital policies on financial assistance, and to end predatory billing and collection practices. We also provide a platform for people who have medical debt to share their experiences, which helps to shape policies aimed at reducing and eliminating medical debt.
The Hospital Equity and Accountability Project
The Hospital Equity and Accountability Project (HEAP) is an effort designed to address the negative impact of hospital and health industry consolidation on systemically excluded communities — including Asian, Black, Indigenous, Latinx, and Pacific Islander communities, immigrants, women, LGBTQ+ people, people with disabilities, older adults, and rural residents. For this project, we collaborate with a cross-movement, national strategic working group on religious health restrictions as well as conduct state-specific work in New York.