Organizing for Outreach
Signing up for health insurance—whether through Medicaid or the Marketplace—can be intimidating, confusing, and stressful. And many people may simply not know that they are eligible for the financial assistance that’s available as part of these coverage programs. That’s why Community Catalyst has a program called Organizing for Outreach, focused on building partnerships with community-based organizations to connect with people who are more likely to be or become uninsured and help make the enrollment process much easier.
By teaming up with existing groups that are embedded in communities—including national, state, and local organizations that excel in power building and community outreach efforts—we’re able to reach people who are uninsured and inadequately-insured to make sure they know what kind of coverage they may be eligible for, and help them get enrolled.
We support on-the-ground outreach, offer tailored messages and resources, and bring partners together from across the country to discuss organizing and education strategies, successes, and challenges. We also share people’s experiences about health insurance enrollment with key policymakers, including the Biden administration. This creates an important feedback loop that demonstrates the national need for sustained and enhanced enrollment assistance.
One of our current priorities focuses on communities that are most likely to be impacted by the end of the Public Health Emergency (PHE)— initiated by the federal government at the onset of COVID-19—which allowed people to maintain their Medicaid coverage without re-enrolling.
We’re also raising awareness about new financial assistance when looking for health care plans in the Marketplace because of the extension of enhanced tax credits and changes to the family glitch rule. (In the past, a family’s eligibility for premium subsidies—in the form of tax credits—depended on whether the employer-based insurance they were offered was affordable at the cost to cover only the employee, no matter how much more expensive premiums would be to cover the whole family. Now, if the employer-based coverage offered will cost more than 9.12 percent of the household income to cover all family members, the employer-based coverage will be considered “unaffordable” and the employee’s family members will be newly eligible for premium tax credits to help cover their costs.)
Most of our work is in communities with high numbers of uninsured people, including: Asian communities, Black communities, Latinx communities, Pacific Islander communities, immigrants, people who identify as LGBTQ+, people with disabilities, rural communities, people with low-incomes, and people with intersectional identities that span various communities.
Our 21 community partners are essential in helping people learn about their coverage options and sign up for the health coverage they need. These groups design and implement outreach and education strategies in communities to bring awareness about health coverage options and available enrollment assistance.
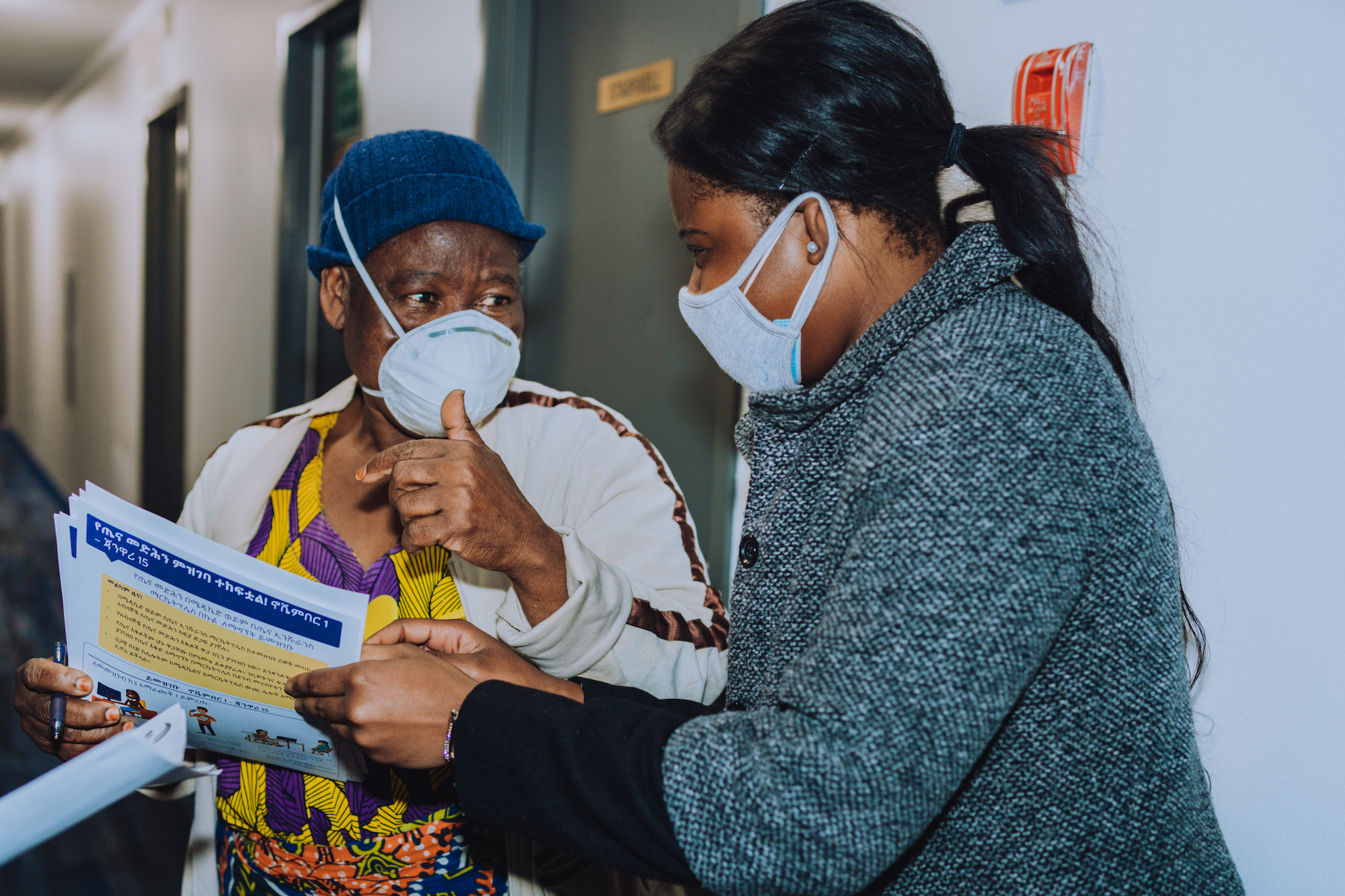
Partner Spotlight: African Communities Together
Mr. A is a 25 year-old African immigrant living in Virginia who works as a waiter and makes minimum wage. Mr. A wanted to sign up for health insurance, but worried about whether he could afford it. When a friend told Mr. A about the enrollment assistance offered by African Communities Together, a Community Catalyst partner, he called to seek help. Mr. A was relieved to speak with another African who understood the dynamics of being an immigrant and applying for Medicaid. Even though he is a green card holder, Mr. A was concerned about answering some of the questions on the enrollment portal regarding his social security number. Mr. A appreciated having someone walk him through the process, explain why his social security number was requested, and how it would be used. Without African Communities Together, Mr. A may not have obtained health insurance.
Visit Organizing for Outreach's online hub for customizable resources
Visit Organizing for Outreach's online hub for customizable resources (Opens in new tab)